Effects of olive oil on blood pressure: A systematic review and meta-analysis
F. Zamora-Zamoraa,*, J.M. Martínez-Galianob,c, J.J. Gaforioc,d,e,f and M. Delgado-Rodríguezb,c
aPaediatric Emergency Department, Hospital Complex of Jaén. Av. del Ejército Español 10; 23007 Jaén, Spain
bDepartment of Health Sciences, Faculty of Experimental Sciences, University of Jaén, Campus las Lagunillas s/n; 23071 Jaén, Spain
cCIBER-ESP, Instituto de Salud Carlos III, C/ Monforte de Lemos 3-5, Pabellón 11, Planta 0, 28029 Madrid, Spain
dCenter for Advanced Studies in Olive Grove and Olive Oils. University of Jaén, Spain
eImmunology Division, Department of Health Sciences, Faculty of Experimental Sciences, University of Jaén, Campus las Lagunillas s/n; 23071 Jaén, Spain
fAgrifood Campus of International Excellence, ceiA3, Spain
*Corresponding author: francisca.zamora.sspa@juntadeandalucia.es
| |
SUMMARY
Hypertension is one of the most important risk factors associated with the development of cardiovascular diseases. Numerous
studies have revealed that a diet enriched in olive oil can have a beneficial effect on blood pressure. This systematic review
includes the effects of olive oil on blood pressure in individuals without previous cardiovascular events. Liquid oil shows
a decrease in blood pressure, while capsules have not produced any effect. Diastolic blood pressure decreased after the consumption
of olive oil, -0.73 mm Hg, 95% CI (-1.07, -0.40); p < 0.001, I2 = 86.9%, with high heterogeneity among the included studies. This reduction was mainly due to extra virgin olive oil (EVOO)
from 10 ml to 50 ml/day: -1.44 mm Hg, 95% CI (-1.89, -1.00); p < 0.001. Regarding systolic blood pressure the observed decrease
is not statistically significant. Further studies on the consumption of EVOO are needed to confirm these results.
|
| |
RESUMEN
Efectos del aceite de oliva en la presión arterial: revisión sistemática y metaanálisis. La hipertensión es uno de los factores de riesgo más importantes asociados con al desarrollo de enfermedades cardiovasculares.
Numerosos estudios han revelado que una dieta enriquecida en aceite de oliva puede producir un efecto beneficioso sobre la
tensión arterial. En esta revisión sistemática se recogen los efectos del aceite de oliva sobre la tensión arterial en individuos
sin eventos cardiovasculares previos. Es el aceite líquido el que ha mostrado los beneficios, mientras que las cápsulas no
han producido ningún efecto. La tensión arterial diastólica disminuyó después del consumo de aceite de oliva, -0.73 mm Hg,
IC 95% (-1.07, -0.40); p < 0.001, I2 = 86.9%, con elevada heterogeneidad entre los estudios incluidos. Esta reducción se debió principalmente al aceite de oliva
virgen extra (AOVE) de 10 ml a 50 ml / día: -1.44 mm Hg, IC 95% (-1.89, -1.00); p < 0.001. En lo que se refiere a la tensión
arterial sistólica el descenso producido no ha sido estadísticamente significativo. Se necesitan más estudios sobre el consumo
de AOVE para confirmar estos resultados.
|
1. INTRODUCTIONTOP
Hypertension is one of the most important risk factors associated with the development of cardiovascular disease. The threshold
for the diagnosis of hypertension is a systolic blood pressure (SBP) of at least 140 mm Hg, a diastolic blood pressure (DBP)
of at least 90 mm Hg, or both (Poulter et al., 2015). Hypertension increases the risk of stroke, coronary heart disease, sudden death, heart failure and peripheral arterial
disease (Mancia et al., 2013). A change in lifestyle can be an effective intervention to control blood pressure. The preventive measures to adopt are
restriction of salt in the diet, moderation in alcohol consumption, abundant fruit consumption, control of weight, regular
physical activity, and smoking cessation (Dickinson et al., 2006).
Several epidemiological studies have analyzed the relationship between monounsaturated fatty acid (MUFA) consumption, such
as olive oil, and hypertension (Alonso et al., 2006). In 2005, the OmniHeart study compared three diets: one rich in carbohydrates, another rich in vegetable proteins, and the
third with MUFA. The diets rich in vegetable proteins and MUFA compared with the carbohydrate diet reduced blood pressure
and improved the lipid profile (Appel et al., 2005). The International Study of Macro/Micronutrients and Blood Pressure (INTERMAP) is a multicenter cross-sectional study of
4680 men and women in which linear regression analyses showed a significant inverse relationship between total MUFA intake
and DBP. A Spanish study showed that the consumption of vegetable oleic acid, with a daily intake of 13 g/day, was associated
with a decrease in SBP (-0.70 mmHg) and DBP (-0.57mm Hg) (Miura et al., 2013). In the PREDIMED (Prevención con Dieta Mediterránea) clinical trial both SBP and DBP decreased 2.3 and 1.2 mm Hg, respectively,
after one year of follow-up (Doménech et al., 2014).
The consumption of olive oil is very common in Mediterranean countries. It is associated with the Mediterranean diet and it
is not clear whether the effects of olive oil are due to the oil itself or to the whole diet pattern. The objective of this
study is to assess whether the consumption of olive oil reduces blood pressure in adults without previous cardiovascular events.
2. METHODSTOP
2.1. DesignTOP
We carried out a systematic review and meta-analysis following the recommendations established by the PRISMA statement (Preferred
Reporting Items for Systematic Reviews and Meta-Analyzes) (Moher et al., 2009). A systematic review protocol was developed, not registered a priori, and not modified after the beginning of the review
process.
2.2. Eligibility criteriaTOP
We used the following inclusion criteria: a) participants: adult population with at least 18 years of age without previous
cardiovascular events; b) intervention: diet enriched with olive oil for at least 12 weeks vs. diet enriched with other fat;
c) outcome measures: SBP or DBP; d) design of included studies: randomized controlled trials (RCTs). We have included both
healthy individuals with cardiovascular risk factors or with other non-cardiovascular pathology.
2.3. Exclusion criteriaTOP
We exclude studies in which the intervention was carried out in cardiovascular patients because they experience a profound
change in their lifestyle, including diet, not comparable with healthy subjects or with other types of diseases. Animal studies
were discarded.
2.4. Research methodsTOP
The following electronic databases were searched from their inception through April 10, 2018: PubMed, Embase, Cochrane plus,
Web of Science, Ovid, Scopus, VHL, TDR. The language of publication was not restricted.
The search strategy was carried out through the combination of keywords related to olive oil intake (olive oil), and the different
expected results: hypertension (arterial pressure, hypertension, blood pressure, DBP, SBP), and the design of adequate studies
for inclusion (randomized controlled trial, systematic review, meta-analysis). Reference lists of identified original articles
were searched manually. Table 1 shows the search strategy for the databases.
TABLE 1. Search strategy
| PubMed, Web of Science, Embase, Ovid, Biblioteca Cochrane plus, Scopus, VHL, TDR |
| 1. olive oil |
| 2. Arterial Pressure |
| 3. Hypertension |
| 4. Blood Pressure |
| 5. Diastolic Pressure |
| 6. Systolic Pressure |
| 7. 2# OR 3# OR 4# OR 5# OR 6# |
| 8. 1# AND 7# |
| 9. 8# AND (Randomized Controlled Trial OR systematic review OR Meta-Analysis) |
| 10. 9# AND humans |
| VHL |
| 1. olive oil |
| 2. hypertension |
| 3. Humans |
| 4. 1# AND 2# AND 3# |
2.5. Risk of bias in individual studiesTOP
We used the Cochrane risk of bias tool to assess risk of bias within the following domains: selection bias, performance bias,
detection bias, attrition bias, reporting bias, and other bias (Higgins and Green, 2011). Table 2 shows the studies after the validity analysis.
Table 2. Characteristics of studies included in the systematic review
| Studies |
Country |
Design |
Duration of intervention |
Participants |
Treatment group |
Control group |
Outcomes Treatment group |
Outcomes Control group |
| Kristensen et al., 2016 |
Denmark |
Double-blind RCT |
24-week |
Psoriatic arthritis |
Capsules 3 g olive oil /day N = 60 |
Capsules 3 g n-3 PUFA / N = 68 |
SBP decrease DBP decrease |
SBP decrease DBP decrease |
| Rozati et al., 2015 |
USA |
RCT |
3 months |
Overweight and obese |
Extra virgin olive oil 39±7g/ day +American diet N = 20 |
Corn oil, soybean oil and butter: 41 ± 8 g / day plus American diet N = 21 |
SBP decrease DBP decrease |
SBP without change DBP decrease |
| Lee et al., 2015 |
South Korea |
Double-blind RCT |
12 weeks |
Diabetic nephropathy |
3 g olive oil / N = 8 |
Omega-3 FA: 3 g / day / N=11 |
SBP decrease DBP without change |
SBP increase DBP decrease |
| Venturini et al., 2015 |
Brazil |
RCT |
90 days |
Metabolic syndrome |
10 ml extra virgin olive oil /day N = 13 |
Usual diet / N = 42 |
SBP decrease DBP decrease |
SBP increase DBP decrease |
| Ceriello et al., 2014 |
Spain |
RCT |
3 months |
Diabetics type II |
Extra virgin olive oil 50 ml /day /N = 12 |
Low fat diet/ N = 12 |
SBP decrease DBP increase |
SBP decrease DBP decrease |
| Toledo et al., 2013 |
Spain |
RCT |
4 years |
Diabetic or ≥ 3 cardiovascular risk factors |
Mediterranean diet + extra virgin olive oil 50 ml /day N = 2441 |
Low-fat diet / N = 2350 |
SBP decrease DBP decrease |
SBP decrease DBP decrease |
| Singhal et al., 2013 |
United Kingdom |
Double blind RCT |
16 weeks |
No diabetics or chronically ill |
Capsules 4g / day olive oil / N = 162 |
4 g (microalgae + palmitic acid) / N = 162 |
SBP decrease DBP decrease |
SBP decrease DBP decrease |
| Tapsell et al., 2013 |
Australia |
RCT |
1 year |
Non-diabetic obesity |
Hypocaloric diet + 1g olive oil /day N = 37 |
Hypocaloric diet + fish + DHA and EPA / N = 38 |
SBP decrease DBP decrease |
SBP decrease DBP increase |
| Konstantinidou et al., 2010 |
Spain |
RCT |
3 months |
Healthy adults |
Mediterranean diet + extra virgin olive oil / N = 30 |
Habitual diet / N = 29 |
SBP decrease DBP increase |
SBP increase DBP increase |
| Taylor et al., 2006 |
United Kingdom |
Double-blind RCT |
12 weeks |
Overweight |
Olive oil 54 cal /day Capsules N = 19 |
Conjugated linoleic acid 4.5 g / d; 60 cal /day Capsules / N = 21 |
SBP increase DBP decrease |
SBP decrease DBP increase |
| Rasmussen et al., 2006 |
Finland, Denmark; Italy; Australia; Sweden |
RCT |
3 months |
Healthy adults |
Olive oil capsules 3.6g/day + MUFA diet N = 19 |
Fish oil capsules 3.6g + MUFA diet /N = 21 |
SBP decrease DBP decrease |
SBP decrease DBP decrease |
| Olsen et al., 2000 |
Denmark, United Kingdom;Sweden;Italy; Netherlands;Belgium; Russia;Norway |
Double-blind RCT |
20 weeks |
Pregnant |
4g Olive oil capsules / day. Group Hypertension induced by pregnancy N = 202 Twin pregnancy group N = 290 |
4 capsules of fish oil Group Hypertension induced by pregnancy N = 184 Twin pregnancy group N = 289 |
DBP increase |
DBP increase |
| Ferrara et al., 2000 |
Italy |
Double-blind crossover |
1 year |
Hypertensive |
Extra virgin olive oil 40g Men and 30 g women /day N = 23 |
Sunflower oil / 40 g men and 30 g women/day N = 23 |
SBP decrease DBP decrease |
SBP increase DBP without change |
| Prisco et al., 1998
|
Italy |
Double blind RCT |
4 months |
Hypertensive |
4g olive oil / day + Mediterranean diet / N = 8 |
4gr EPA and DHA/day + Mediterranean diet / N = 8 |
SBP without change DBP without change |
SBP decrease DBP decrease |
| Bonnema et al., 1995 |
Denmark |
Double-blind RCT |
6 months |
Diabetics with incipient nephropathy |
Olive oil 6 g in capsules / N = 14 |
6 g in fish oil capsules/ N = 14 |
SBP increase DBP increase |
SBP decrease DBP decrease |
| Cal/d: calories/day; DBP: diastolic blood pressure; DHA: docosahexaenoic acid; EPA: eicosapentaenoic acid; FA: fatty acid; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids; RCT: randomized controlled trial; SBP: systolic blood pressure. |
2.6. Data extraction and managementTOP
Two researchers made the selection of articles independently. Discrepancies were discussed with a third review author until
consensus was reached. The following data were extracted from each study: authors, year of publication, country of implementation,
duration, amount of olive oil intake in the experimental group and fat in the control one, characteristics and number of participants
in each intervention applied, SBP and DBP (Table 2).
2.7. Data synthesisTOP
The outcome parameter was the change in blood pressure regarding baseline values; the mean standard error of the change was
computed. Mean differences (MDs) were pooled using a fixed effects model. Heterogeneity between studies results was tested
using the Q test. The proportion of heterogeneity was quantified with the I2 parameter. I2 > 50 % was considered to represent considerable heterogeneity. Metarregression was performed to explore the causes of heterogeneity.
We applied Egger’s method to determine the possible existence of publication bias. All data were analyzed using Stata 14 SE
program (College Station, TX, USA).
3. RESULTSTOP
3.1. Literature researchTOP
The search identified 872 studies, 687 of which were identified in different databases: 119 in PubMed, 23 in Embase, 32 in
the Cochrane Plus Library, 167 in the Web of Science, 35 in Ovid, 232 in Scopus, and 79 in VHL; while 185 were located through
the grey literature of TDR and hand searched for references. After the exclusion of duplicates, 691 studies were evaluated.
27 studies were reviewed in full text, and 15 studies were finally included. The reasons for exclusion are detailed in Figure 1.
|
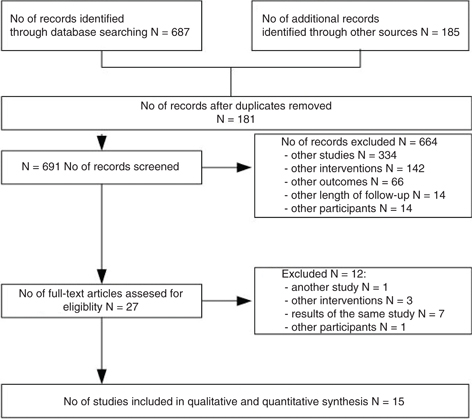 Figure 1. Flow chart of study procedure. Randomized controlled studies of at least three months duration, not developed in animals, or in individuals with previous cardiovascular events have been included. Other interventions have been excluded, such as the administration of other non-ingested supplements or the intake of two oils together at the same time. Figure 1. Flow chart of study procedure. Randomized controlled studies of at least three months duration, not developed in animals, or in individuals with previous cardiovascular events have been included. Other interventions have been excluded, such as the administration of other non-ingested supplements or the intake of two oils together at the same time.
|
|
3.2. Characteristics of studies included in systematic reviewTOP
Fifteen studies were included in the systematic review and meta-analysis (Kristensen et al., 2016, Rozati et al., 2015, Lee et al., 2015, Venturini et al., 2015, Ceriello et al., 2014, Toledo et al., 2013, Singhal et al., 2013, Tapsell et al., 2013, Konstantinidou et al., 2010, Taylor et al., 2006, Rasmussen et al., 2006, Olsen et al., 2000, Ferrara et al., 2000, Prisco et al., 1998, Bonnema et al., 1995). Table 2 shows a summary of the information extracted from the included studies. The designs used by the studies were: double blind
parallel RCTs (Kristensen et al., 2016, Lee et al., 2015, Singhal et al., 2013, Taylor et al., 2006, Olsen et al., 2000, Prisco et al., 1998, Bonnema et al., 1995), double-blind, randomized crossover study (Ferrara et al., 2000), and non-blinded RCTs (Rozati et al., 2015, Venturini et al., 2015, Ceriello et al., 2014, Toledo et al., 2013, Tapsell et al., 2013, Konstantinidou et al., 2010, Rasmussen et al., 2006). The follow-up ranged from 12 weeks to 4 years. The countries in which the studies were developed were Spain (Ceriello et al., 2014, Toledo et al., 2013, Konstantinidou et al., 2010), Denmark (Kristensen et al. 2016, Bonnema et al.,1995), Italy (Ferrara et al., 2000, Prisco et al., 1998), United Kingdom (Singhal et al., 2013, Taylor et al., 2006), South Korea (Lee et al., 2015), USA (Rozati et al., 2015), Brazil (Venturini et al., 2015), Australia (Tapsell et al., 2013), and two multinational studies: Denmark, United Kingdom, Sweden, Italy, Netherlands, Belgium, Russia and Norway (Olsen et al., 2000); and Finland, Denmark, Italy, Australia and Sweden (Rasmussen et al., 2006).
The fifteen studies included 6651 participants: 3358 had ingested olive oil and 3293 were fed the control diet. Four studies
had more than two arms; in these studies the following branches were discarded for the present review: in the PREDIMED study
the branch with Mediterranean diet plus nuts (Toledo et al., 2013), refined olive oil (Konstantinidou et al., 2010), hypocaloric diet plus fish (Tapsell et al., 2013), and pregnant women with fewer weeks of administration (Olsen et al., 2000). Venturini et al., (2015) gives their outcomes as mean and interquartile range and they could not be included in meta-analysis. Men and women were
pooled in the analyses.
The participants were adults without cardiovascular events. Some participants had cardiovascular risk factors such as overweight
or obesity (Rozati et al., 2015, Tapsell et al., 2013, Taylor et al., 2006), diabetes mellitus (Ceriello et al., 2014), incipient or established diabetic nephropathy (Lee et al., 2015, Bonnema et al., 1995) or more than three cardiovascular risk factors (Toledo et al., 2013), hypertension (Ferrara et al., 2000, Prisco et al., 1998), metabolic syndrome (Venturini et al., 2015) and psoriatic arthritis (Kristensen et al., 2016). Three studies were performed in healthy adults (Singhal et al., 2013, Konstantinidou et al., 2010, Rasmussen et al., 2006). Olsen et al., (2000) recruited twin pregnancies and pregnancy induced hypertension.
3.3. Types of interventionsTOP
The olive oil was administered in capsules of 1-6 g/day (Kristensen et al., 2016, Lee et al., 2015, Singhal et al., 2013, Tapsell et al., 2013, Taylor et al., 2006, Rasmussen et al., 2006, Olsen et al., 2000, Prisco et al., 1998, Bonnema et al., 1995), and in liquid form as extra virgin olive oil (EVOO) from 10 ml to 50 ml/day (Rozati et al., 2015, Venturini et al., 2015, Ceriello et al., 2014, Toledo et al., 2013, Ferrara et al., 2000, Konstantinidou et al., 2010), in the context of different types of diets, such as the American diet (Rozati et al., 2015), or the Mediterranean diet (Konstantinidou et al., 2010, Toledo et al., 2013, Prisco et al., 1998). The studies that supplemented liquid oil provided it as EVOO, while the studies with capsule supplement provided it with
olive oil.
The control groups took both capsules, liquid oil, habitual diet and low-fat diet. The controls took capsules with different
fatty acids: microalgae and palmitic acid (Singhal et al., 2013), conjugated linoleic acid (Taylor et al., 2006), docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) (Kristensen et al., 2016, Lee et al., 2015, Tapsell et al., 2013, Bonnema et al., 1995, Rasmussen et al., 2006, Olsen et al., 2000, Prisco et al., 1998). In liquid form the next fats were administered to the control groups: corn oil, soybean oil and butter (Rozati et al., 2015), and sunflower oil (Ferrara et al., 2000). Finally, in four studies, no supplement was provided to the control groups: habitual diet (Venturini et al., 2015, Konstantinidou et al., 2010), and low fat diet (Ceriello et al., 2014, Toledo et al., 2013).
The diet administered was adequate to the energy requirements, except in Tapsell et al., (2013) who administered a hypocaloric diet with 1750 (SD 417) kcal and 1600 (SD 355) kcal in the olive oil and control groups, respectively.
Physical activity was not restricted in the included studies; they were requested to maintain their regular routine of physical
activity. Tapsell et al., (2013), recommended walking for 30-minutes three days a week, with similar results among groups.
3.4. Outcome measuresTOP
Fourteen studies assessed DBP and SBP, and one study only DBP (Olsen et al., 2000). No adverse events were mentioned: only nine participants in the n-3 polyunsaturated fatty acid (PUFA) supplemented group
and six participants in the olive oil group reported mild gastrointestinal adverse effects in Kristensen et al., (2016).
3.5. Risk of bias in individual studiesTOP
We used the Cochrane risk of bias tool (Higgins and Green, 2011) to assess all studies for their risk of bias within the following domains: selection bias, performance bias, detection bias,
attrition bias, reporting bias, and other bias. Figure 2 provides an overview of the risk of bias assessment. Two studies had high risk for selective reporting bias (Venturini et al., 2015, Olsen et al., 2000) and one study was classified as high risk for attrition bias (Tapsell et al., 2013). An intention-to-treat analysis was performed. The included studies were considered as having low risk for bias.
|
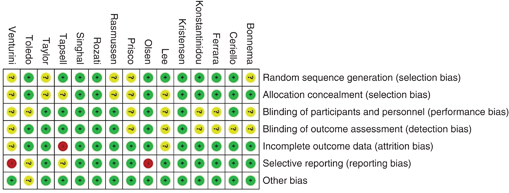 Figure 2. Risk of bias. For each study, each domain of bias is indicated as: low risk of bias in green, unclear risk of bias in yellow, and high risk of bias, in red. Figure 2. Risk of bias. For each study, each domain of bias is indicated as: low risk of bias in green, unclear risk of bias in yellow, and high risk of bias, in red.
|
|
3.6. Results of the meta-analysisTOP
Olive oil did not decrease SBP more than other fat, MDs = -0.11, CI 95 % (-0.68, 0.46), I2 = 85.1%; p heterogeneity < 0.001. The studies dispensed liquid olive oil or capsules. To identify the effect of the two kinds of supplementation
meta-analysis was stratified by this variable (capsules and oil) (Figure 3): no significant effect was observed either for capsules or liquid on SBP.
|
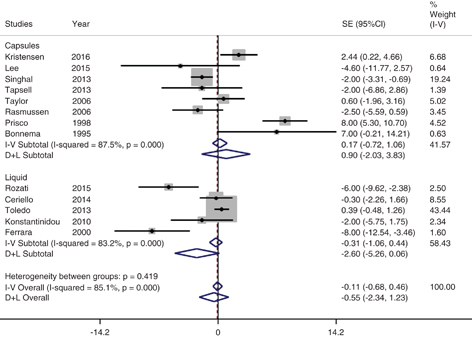 Figure 3. Meta-analysis of the effect of olive oil on systolic blood pressure, stratified by type of supplementation. The mean standard error of the change was computed. For each study, the shaded square represents the point estimate of the intervention effect. The individuals who have taken olive oil are located to the left of the forest plot. Figure 3. Meta-analysis of the effect of olive oil on systolic blood pressure, stratified by type of supplementation. The mean standard error of the change was computed. For each study, the shaded square represents the point estimate of the intervention effect. The individuals who have taken olive oil are located to the left of the forest plot.
|
|
Olive oil showed a significant decrease in DBP with a fixed effects model of -0.73 mm Hg, 95% CI (-1.07, -0.40); p < 0.001; I2 = 84.5%; p heterogeneity < 0.001. This effect was mainly due to liquid oil EVOO: a reduction of -1.44 mm Hg, 95% CI (-1.89, -1.00);
p < 0.001; with a high heterogeneity, I2 = 86.9%; p heterogeneity < 0.001. The olive oil in capsules had no significant influence on DBP, 0.14 mm Hg, 95% CI (-0.35, 0.64), I2 = 76.2%, p = 0.5 (Figure 4). A meta-regression was performed to inquire the causes of heterogeneity. Neither the quantity of grams of olive oil on SBP
(p = 0.35) or DBP (p = 0.51), nor the year of publication (p = 0.27 and p = 0.70, respectively), seem to be the cause of the heterogeneity found among the studies selected for the meta-analysis.
Among the causes of heterogeneity are the different diets, and the characteristics of the patients for whom the studies were
developed.
|
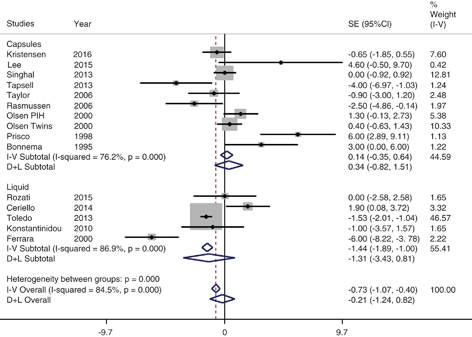 Figure 4. Meta-analysis of olive oil on diastolic blood pressure, stratified by type of supplementation. The mean standard error of the change was computed. For each study, the shaded square represents the point estimate of the intervention effect. The individuals who have taken olive oil are located to the left of the forest plot. Figure 4. Meta-analysis of olive oil on diastolic blood pressure, stratified by type of supplementation. The mean standard error of the change was computed. For each study, the shaded square represents the point estimate of the intervention effect. The individuals who have taken olive oil are located to the left of the forest plot.
|
|
3.7. Risk of bias across studies (publication bias)TOP
Egger’s method showed p values of 0.67 and 0.23 for SBP and DBP, respectively.
4. DISCUSSIONTOP
In this systematic review of 6651 participants without previous cardiovascular events in 15 RCTs, comparing a diet enriched
with olive oil versus a diet enriched with other fats, a significant reduction in DBP was observed, with high heterogeneity.
This heterogeneity may be due to differences in the diets of control groups, characteristics of the populations (very different
countries, with different risk factors, etc.), and the type of supplementation of olive oil. The EVOO seems to be the main
factor responsible for the decrease in DBP. The PREDIMED trial (Toledo et al., 2013) is the more influential study in the pooled results with a weight of 43.44% and 46.57% for SBP and DBP, respectively, and
with more of the 70% of all subjects. The use of a random effects model implies giving a higher weight for much smaller studies,
and more prone to bias than the PREDIMED. That is the reason we relied on the fixed effects model.
Considering the individual studies, a higher decrease in SBP was obtained with liquid EVOO, about 40 g in men and 30 g in
women, compared to sunflower oil (Ferrara et al., 2000): -8 mm Hg in SBP, CI 95% (-12.5, -3.46), and -6 mm Hg in DBP, CI 95% (-8.22, -3.78). In another study (Rozati et al., 2015), EVOO (39 ± 7 g/day) significantly reduced SBP in -6 mm Hg, 95% CI (-9.62,-2.38), when compared with corn oil, soybean oil
and butter together in an American diet. A lower reduction was observed with olive oil capsules (4 g) versus capsules of microalgae
and palmitic acid: -2 mm Hg in SBP, 95% CI (-3.31, -0.69) (Singhal et al., 2013). In the PREDIMED trial after 3.8 years of follow-up (Toledo et al., 2013), liquid EVOO decreased DBP by -1.53 mm Hg, 95% CI (-2.01, -1.04). This reduction is similar to that found with olive oil
capsules, compared to capsules containing fish oil (Rasmussen et al., 2006), -2.5 mm Hg in DBP, 95% CI (-4.86, -0.14), and lower than reported in obese subjects (Tapsell et al., 2013): -4 mm Hg in DBP, 95% CI (-6.97, -1.03).
The study by Venturini et al., (2015), which could not be pooled as a mean difference could not be obtained, observed interesting results comparing EVOO with a
regular diet in participants with metabolic syndrome. They reported a decrease in the mean SBP of -5 mm Hg and -14 mm Hg in
DBP.
Other studies with interventions of shorter duration than 12 weeks, not included in this review, showed significant reductions
in blood pressure. In a double-blind crossover trial of 24 women, Moreno Luna et al., (2012) examined the influence of oil with high content in polyphenols on blood pressure: EVOO reduced SBP by -7.91 ± 9.51 mm Hg
and DBP -6.65 ± 6.63 mm Hg. These effects are similar to those observed in a systematic review on the effect of first-line
antihypertensive drugs choice (Wright and Musini, 2009). The effect of polyphenols has also been evaluated in a group of 160 healthy men from the North, Center and South of Europe
(Bondia-Pons et al., 2007) in a randomized cross-over trial with three intervention periods: 25 ml/day of olive oil were administered with different
concentrations of polyphenols. Both SBP and DBP decreased after consuming olive oil for nine weeks. In addition, the properties
of virgin olive oil were evaluated in the SOLOS study in 40 men with stable coronary disease (Fitó et al., 2005): SBP decreased after the intake of EVOO (p < 0.001), with no change in DBP. A systematic review on the effects of virgin
olive oil polyphenols found significant differences in SBP and no effect on DBP (Hohmann et al., 2015), although the number of pooled subjects is small, 69.
Olive oil seems to inhibit the activity of angiotensin-converting enzymes, and blocks the binding to angiotensin II receptor,
and this hypotensive activity was demonstrated in studies on animals or humans (Patten et al., 2016).
Among the strengths of this study is the exhaustive search developed without language restriction, the number of studies reviewed,
and the quality of the included studies. The results could be extended to healthy subjects, with cardiovascular risk factors,
type 2 diabetes, hypertension, overweight, obesity, and countries with distinct economic and social development. The main
limitation of our systematic review is the heterogeneity among the studies. It could be justified because some studies have
been carried out in areas with regular consumption of olive oil and it is possible that the group control has also taken olive
oil. In addition, some participants have taken antihypertensive treatment for their underlying disease, thus decreasing the
potential benefit of olive oil. Toledo et al., 2013, developed a study on individuals with different cardiovascular risk factors, including hypertension for which they need
antihypertensive therapy, although the individuals were distributed into similar percentages between the intervention and
control groups, 1666 (68%) patients in the extra virgin olive oil group and 1666 (70.9%) in the control group. Likewise, in
Ferrara et al., 2000, did a randomized crossover study in which there were basic conditions for all individuals. At the end of the follow-up,
daily drug dosage was significantly reduced in the EVOO group, and 34.7% needed no antihypertensive therapy, while all patients
required treatment during the sunflower oil diet. Physical activity may also vary among different populations.
Nevertheless, we consider that the number of studies on olive oil and blood pressure is still small. The intake of EVOO of
between 10-50 ml per day can reduce diastolic blood pressure in healthy individuals or those with cardiovascular risk factors,
even in hypertensive patients, and can be an important therapeutic tool. Further studies on EVOO are needed to reduce heterogeneity
and consolidate the results.
5. CONCLUSIONSTOP
The present meta-analysis provides evidence for a beneficial effect of EVOO on blood pressure in participants without cardiovascular
events. Healthy individuals or those with cardiovascular risk factors can benefit from a reduction in DBP if they consume
olive oil for at least three months.
REFERENCESTOP
| ○ |
Alonso A, Ruiz-Gutiérrez V, Martínez-González MA. 2006. Monounsaturated fatty acids, olive oil and blood pressure: epidemiological,
clinical and experimental evidence. Public Health Nutr. 9, 251–257. https://doi.org/10.1079/PHN2005836 |
| ○ |
Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER 3rd, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, Charleston
J, McCarron P, Bishop LM; OmniHeart Collaborative Research Group. 2005. Effects of protein, monounsaturated fat, and carbohydrate
intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 294, 2455–2564. https://doi.org/10.1001/jama.294.19.2455 |
| ○ |
Bondia-Pons I, Schroder H, Covas MI, Castellote AI, Kaikkonen J, Poulsen HE, Gaddi AV, Machowetz A, Kiesewetter H, Lopez-Sabater
MC. 2007. Moderate consumption of olive oil by healthy European men reduces systolic blood pressure in non-Mediterranean participants.
J. Nutr. 137, 84–87. https://doi.org/10.1093/jn/137.1.84 |
| ○ |
Bonnema SJ, Jespersen LT, Marving J, Gregersen G. 1995. Supplementation with olive oil rather than fish oil increases small
arterial compliance in diabetic patients. Diabetes Nutr. Metab. 8, 81–87.
|
| ○ |
Ceriello A, Esposito K, La Sala L, Pujadas G, De Nigris V, Testa R, Bucciarelli L, Rondinelli M, Genovese S. 2014. The protective
effect of the Mediterranean diet on endothelial resistance to GLP-1 in type 2 diabetes: a preliminary report. Cardiovasc. Diabetol. 13, 140. https://doi.org/10.1186/s12933-014-0140-9 |
| ○ |
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, Williams B, Ford GA. 2006. Lifestyle interventions to
reduce raised blood pressure: a systematic review of randomized controlled trials. J. Hypertens. 24, 215–233. https://doi.org/10.1097/01.hjh.0000199800.72563.26 |
| ○ |
Doménech M, Roman P, Lapetra J, García de la Corte FJ, Sala-Vila A, de la Torre R, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez
V, Lamuela-Raventós RM, Toledo E, Estruch R, Coca A, Ros E. 2014. Mediterranean diet reduces 24-hour ambulatory blood pressure,
blood glucose, and lipids: one-year randomized, clinical trial. Hypertension 64, 69–76. https://doi.org/10.1161/HYPERTENSIONAHA.113.03353 |
| ○ |
Ferrara LA, Raimondi AS, d’Episcopo L, Guida L, Dello Russo A, Marotta T. 2000. Olive oil and reduced need for antihypertensive
medications. Arch. Intern. Med. 160, 837–842. https://doi.org/10.1001/archinte.160.6.837 |
| ○ |
Fitó M, Cladellas M, de la Torre R, Marti J, Alcántara M, Pujadas-Bastardes M, Marrugat J, Bruguera J, Lopez-Sabater MC, Vila
J, Covas MI; members of the SOLOS Investigators. 2005. Antioxidant effect of virgin olive oil in patients with stable coronary
heart disease: a randomized, crossover, controlled, clinical trial. Atherosclerosis 181, 149–158. https://doi.org/10.1016/j.atherosclerosis.2004.12.036 |
| ○ |
Higgins JPT, Green S (editors). 2011. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March
2011]. The Cochrane Collaboration.
|
| ○ |
Hohmann CD, Cramer H, Michalsen A, Kessler C, Steckhan N, Choi K, Dobos G. 2015. Effects of high phenolic olive oil on cardiovascular
risk factors: A systematic review and meta-analysis. Phytomedicine 22, 631–640. https://doi.org/10.1016/j.phymed.2015.03.019 |
| ○ |
Konstantinidou V, Covas MI, Muñoz-Aguayo D, Khymenets O, de la Torre R, Sáez G, Tormos M del C, Toledo E, Marti A, Ruiz-Gutiérrez
V, Ruiz Méndez MV, Fito M. 2010. In vivo nutrigenomic effects of virgin olive oil polyphenols within the frame of the Mediterranean
diet: a randomized controlled trial. FASEB J. 24, 2546–2557. https://doi.org/10.1096/fj.09-148452 |
| ○ |
Kristensen S, Schmidt EB, Schlemmer A, Rasmussen C, Lindgreen E, Johansen MB, Christensen JH. 2016. The effect of marine n-3
polyunsaturated fatty acids on cardiac autonomic and hemodynamic function in patients with psoriatic arthritis: a randomised,
double-blind, placebo-controlled trial. Lipids Health Dis. 15, 216. https://doi.org/10.1186/s12944-016-0382-5 |
| ○ |
Lee SM, Chung SH, Park Y, Park MK, Son YK, Kim SE, An WS. 2015. Effect of Omega-3 Fatty Acid on the Fatty Acid Content of
the Erythrocyte Membrane and Proteinuria in Patients with Diabetic Nephropathy. Int. J. Endocrinol. 2015, 208121. https://doi.org/10.1155/2015/208121 |
| ○ |
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, Backer GD, Dominiczak A, Galderisi
M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA,
Sleight P, Viigimaa M, Waeber B, Zannad F; Grupo de Trabajo para el manejo de la hipertensión arterial de la Sociedad Europea
de Hipertensión (ESH) y la Sociedad Europea de Cardiología (ESC). 2013. Guía de práctica clínica de la ESH/ESC 2013 para el
manejo de la hipertensión arterial. Rev. Esp. Cardiol. 66, e1-e064. https://doi.org/10.1016/j.recesp.2013.07.016 |
| ○ |
Miura K, Stamler J, Brown IJ, Ueshima H, Nakagawa H, Sakurai M, Chan Q, Appel LJ, Okayama A, Okuda N, Curb JD, Rodriguez BL,
Robertson C, Zhao L, Elliott P; INTERMAP Research Group. 2013. Relationship of dietary monounsaturated fatty acids to blood
pressure: the International Study of Macro/Micronutrients and Blood Pressure. J. Hypertens. 31, 1144–1150. https://doi.org/10.1097/HJH.0b013e3283604016 |
| ○ |
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. 2009. Preferred reporting items for systematic reviews and meta-analyses:
the PRISMA statement. PLoS Med. 6, e1000097. https://doi.org/10.1371/journal.pmed.1000097 |
| ○ |
Moreno-Luna R, Muñoz-Hernández R, Miranda ML, Costa AF, Jiménez-Jiménez L, Vallejo-Vaz AJ, Muriana FJ, Villar J, Stiefel P.
2012. Olive oil polyphenols decrease blood pressure and improve endothelial function in young women with mild hypertension.
Am. J. Hypertens. 25, 1299–1304. https://doi.org/10.1038/ajh.2012.128 |
| ○ |
Olsen SF, Secher NJ, Tabor A, Weber T, Walker JJ, Gluud C. 2000. Randomised clinical trials of fish oil supplementation in
high risk pregnancies. Fish Oil Trials in Pregnancy (FOTIP) Team. BJOG 107, 382–395. https://doi.org/10.1111/j.1471-0528.2000.tb13235.x |
| ○ |
Patten GS, Abeywardena MY, Bennett LE. 2016. Inhibition of Angiotensin Converting Enzyme, Angiotensin II Receptor Blocking,
and Blood Pressure Lowering Bioactivity across Plant Families. Crit. Rev. Food Sci. Nutr. 56, 181–214.
|
| ○ |
Poulter NR, Prabhakaran D, Caulfield M. 2015. Hypertension. Lancet 386, 801–812. https://doi.org/10.1016/S0140-6736(14)61468-9 |
| ○ |
Prisco D, Paniccia R, Bandinelli B, Filippini M, Francalanci I, Giusti B, Giurlani L, Gensini GF, Abbate R, Neri Serneri GG.
1998. Effect of medium-term supplementation with a moderate dose of n-3 polyunsaturated fatty acids on blood pressure in mild
hypertensive patients. Thromb. Res. 91, 105–112. https://doi.org/10.1016/S0049-3848(98)00046-2 |
| ○ |
Rasmussen BM, Vessby B, Uusitupa M, Berglund L, Pedersen E, Riccardi G, Rivellese AA, Tapsell L, Hermansen K; KANWU Study
Group. 2006. Effects of dietary saturated, monounsaturated, and n-3 fatty acids on blood pressure in healthy subjects. Am. J. Clin. Nutr. 83, 221–226. https://doi.org/10.1093/ajcn/83.2.221 |
| ○ |
Rozati M, Barnett J, Wu D, Handelman G, Saltzman E, Wilson T, Li L, Wang J, Marcos A, Ordovás JM, Lee YC, Meydani M, Meydani
SN. 2015. Cardio-metabolic and immunological impacts of extra virgin olive oil consumption in overweight and obese older adults:
a randomized controlled trial. Nutr. Metab. (Lond). 12, 28. https://doi.org/10.1186/s12986-015-0022-5 |
| ○ |
Singhal A, Lanigan J, Storry C, Low S, Birbara T, Lucas A, Deanfield J. 2013. Docosahexaenoic acid supplementation, vascular
function and risk factors for cardiovascular disease: a randomized controlled trial in young adults. J. Am. Heart Assoc. 2, e000283. https://doi.org/10.1161/JAHA.113.000283 |
| ○ |
Tapsell LC, Batterham MJ, Charlton KE, Neale EP, Probst YC, O’Shea JE, Thorne RL, Zhang Q, Louie JC. 2013. Foods, nutrients
or whole diets: effects of targeting fish and LCn3PUFA consumption in a 12mo weight loss trial. BMC Public Health 13, 1231. https://doi.org/10.1186/1471-2458-13-1231 |
| ○ |
Taylor JS, Williams SR, Rhys R, James P, Frenneaux MP. 2006. Conjugated linoleic acid impairs endothelial function. Arterioscler. Thromb. Vasc. Biol. 26, 307–312. https://doi.org/10.1161/01.ATV.0000199679.40501.ac |
| ○ |
Toledo E, Hu FB, Estruch R, Buil-Cosiales P, Corella D, Salas-Salvadó J, Covas MI, Arós F, Gómez-Gracia E, Fiol M, Lapetra
J, Serra-Majem L, Pinto X, Lamuela-Raventós RM, Sáez G, Bulló M, Ruiz-Gutiérrez V, Ros E, Sorli JV, Martínez-González MA.
2013. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: results from a randomized controlled trial.
BMC Med. 11, 207. https://doi.org/10.1186/1741-7015-11-207 |
| ○ |
Venturini D, Simão AN, Urbano MR, Dichi I. 2015. Effects of extra virgin olive oil and fish oil on lipid profile and oxidative
stress in patients with metabolic syndrome. Nutrition 31, 834–840. https://doi.org/10.1016/j.nut.2014.12.016 |
| ○ |
Wright JM, Musini VM. 2009. First-line drugs for hypertension. Cochrane Database Syst. Rev. 3, CD001841. https://doi.org/10.1002/14651858.CD001841.pub2 |
Figure 1. Flow chart of study procedure. Randomized controlled studies of at least three months duration, not developed in animals, or in individuals with previous cardiovascular events have been included. Other interventions have been excluded, such as the administration of other non-ingested supplements or the intake of two oils together at the same time.